
Syphilis – Serology
Conformément au Règlement de l’Ontario 671/92 de la Loi sur les services en français, les renseignements d’analyses de laboratoire liés à la présente page ne sont offerts qu’en anglais parce qu’ils sont de nature scientifique ou technique et destinés uniquement à l’usage des fournisseurs de soins de santé qualifiés et non aux membres du public.
This page provides serological testing information for syphilis at Public Health Ontario (PHO). The causative agent of syphilis is Treponema pallidum subsp. pallidum. For information regarding other testing options, refer to the following PHO webpages:
- Syphilis Chancre by direct fluorescence
- Syphilis CSF testing
- Prenatal Serology
Updates:
- Reporting: Due to changes in PHO’s and Ontario’s laboratory information systems, cumulative reporting is no longer available.
Testing Indications
Syphilis serology testing is indicated for routine screening, diagnosis of suspected syphilis infections, and treatment monitoring of syphilis cases. Screening is recommended for individuals presenting with risk factors, and pregnant people in their first trimester or at the first prenatal visit. Repeat screening in pregnancy should be considered for individuals with ongoing or high risk. For more information on syphilis screening, refer to the Canadian Guidelines on Sexually Transmitted Infections.
If ordering as part of a prenatal screening, see Prenatal Serology. For initial syphilis testing in newborns for the investigation of congenital syphilis, it is recommended that maternal serum also be submitted with a separate requisition.
Acceptance/Rejection Criteria
- Donor testing is not available through PHO’s laboratory. Specimens from patients being screened as potential donors (e.g. organ, tissue, cells, fertility, etc.) should be referred to a laboratory that performs donor screening assays. Specimens received for donor screening at PHO’s laboratory will be rejected.
- Specimens received more than 7 days post collection will not be tested.
- Cord blood samples are not acceptable.
Specimen Requirements
| Test Requested | Required Requisition(s) | Specimen Type | Minimum Volume | Collection Kit |
Syphilis serology |
Serum |
1.5 mL |
Serum Separator Tubes (SST) |
Submission and Collection Notes
ALL sections of the General Test Requisition must be completed by authorized health care providers for each specimen submitted, or testing may be delayed or cancelled.
For clinical specimens, label the specimen container(s) with the patient’s first and last name, date of collection, and one other unique identifier such as the patient’s date of birth or Health Card Number. For additional information see: Criteria for Acceptance of Patient Specimens. Failure to provide this information may result in rejection or testing delay.
Public Health Ontario (PHO) prefers centrifuged serum separator tubes for serological testing requests.
Generally only one FULL draw 5 mL SST is needed for testing a combination of up to six infectious disease serology markers. If a full tube cannot be drawn, submit two tubes. Refer to Serology Testing - Laboratory Specimen Collection and Submission Instructions for more information.
Do not submit glass tubes.
Limitations
- Heat-inactivated, hemolysed, icteric, lipemic or microbial contaminated serum is not recommended for testing.
- The screen test may be falsely negative in early infection.
- Liquid anticoagulants may have a dilution effect resulting in lower concentrations for individual patient specimens.
Storage and Transport
Place specimen tube in biohazard bag and seal. Place completed General Test Requisition in the pouch at the front of the biohazard bag.
Specimen tubes should be stored at 2-8°C following collection and centrifugation, and should be shipped to PHO’s laboratory on ice packs within 3 days of collection. If delayed shipping is anticipated, remove serum from clot and store frozen at -20°C or colder, and ship on dry ice.
All clinical specimens must be shipped in accordance to the Transportation of Dangerous Good Act.
Test Frequency and Turnaround Time (TAT)
Syphilis screening is performed daily Monday to Friday.
Syphilis confirmatory testing is performed daily Monday to Friday.
Turnaround time is up to 3 business days from receipt at PHO for non-reactive specimens and up to 6 business days for reactive specimens.
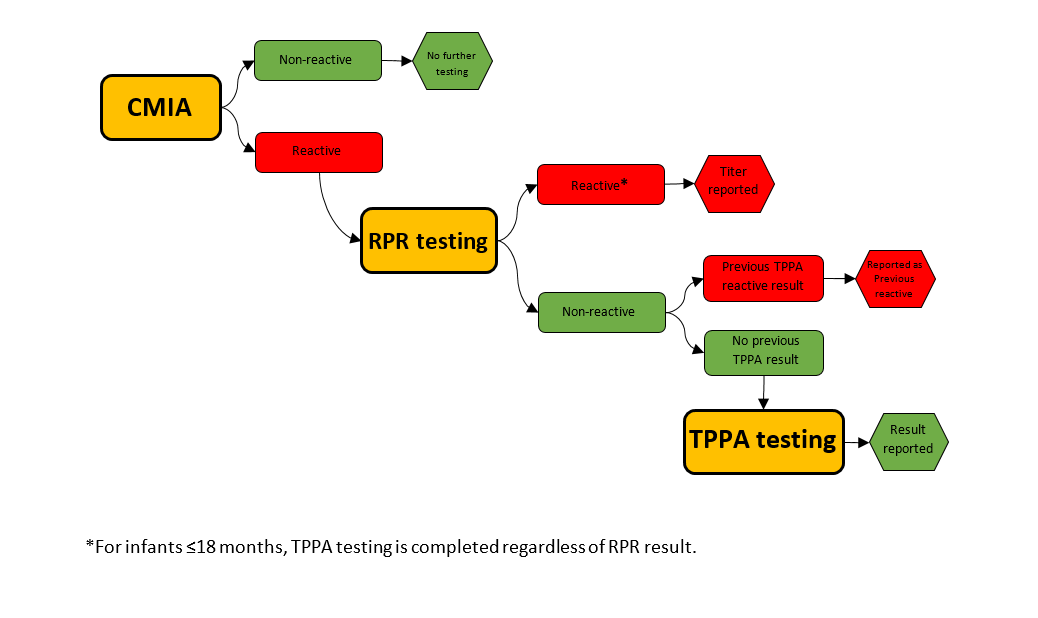
PHO follows a reverse algorithm for syphilis testing.
- Syphilis Screening: Chemiluminescent microparticle immunoassay (CMIA) – a qualitative immunoassay that detects treponemal antibodies (IgG and IgM) to Treponema pallidum. This test does not distinguish between IgG and IgM.
- Syphilis Confirmatory:
- Rapid plasma reagin (RPR) - a semi-quantitative flocculation assay that detects non-treponemal antibodies to cardiolipin-lecithin- cholesterol (Reagin antibodies).
- Treponema pallidum particle agglutination (TP.PA) - a qualitative gelatin particle agglutination assay that confirms antibodies (IgG and IgM) to Treponema pallidum. This test does not distinguish between IgG and IgM. TP.PA reactivity is used as an aid in the diagnosis of current/past syphilis infection.
Algorithm
Serum specimens submitted for syphilis serology are tested following the algorithm below:
Interpretation
Syphilis serology results must be interpreted in the context of the patient’s clinical presentation, risk factors, treatment, and exposure history. Syphilis staging cannot be done with serology results alone. The following table provides interpretations and recommendations for the most common results.
| Serology Screening Test (CMIA)1 | Confirmatory Test (RPR) | Confirmatory Test (TPPA)1 | Possible Interpretations/ Recommendations |
|---|---|---|---|
|
Non-reactive |
Not tested |
Not tested |
|
|
Reactive |
Reactive (titer) |
Not tested |
|
|
Reactive |
Reactive (titer) |
Reactive/ |
|
|
Reactive |
Non-reactive |
Reactive/ |
Patients ≤18 months
|
|
Reactive |
Non-reactive |
Non-reactive |
Patients ≤18 months
|
|
Reactive |
Non-reactive |
Indeterminate |
|
1Maternal antibody can be present in infants for up to 18 months.
2https://cps.ca/en/documents/position/congenital-syphilis
3In general, a four-fold change in RPR titer is considered significant. A four-fold change in titer is equivalent to a change in two dilutions (eg. 1:4 to 1:16).
Reporting
Results are reported to the physician, authorized health care provider (General O. Reg 45/22, s.18), or submitter as indicated on the requisition.
Due to changes in PHO’s and Ontario’s laboratory information systems, cumulative reporting is no longer available.
Specimens that are positive for syphilis are reported to the Medical Officer of Health as per the Ontario Health Protection and Promotion Act.
Vous n'avez pas de compte MonSPO? S'inscrire maintenant

